The final outputs of the Green Social Prescribing Test and Learn Pilot National Evaluation have been published.
Working with researchers at The University of Sheffield, Sheffield Hallam University, and the University of Plymouth we at ECEHH have undertaken an evaluation of the Preventing and Tackling Mental Ill Health through Green Social Prescribing Project (GSP Project), a two year £5.77 million cross-governmental initiative that ran across seven test and learn pilot sites in England (for details see below). The aim of the pilots was to develop the integrated systems and processes relating to the use of nature-based settings and activities to promote wellbeing and improve mental health. The project tested how to embed Green Social Prescribing to:
- Improve mental health outcomes.
- Reduce health inequalities.
- Reduce demand on the health and social care
system. - Develop best practice in making green social activities more resilient and accessible.
You can read the results in the different outputs we produced.
- Final Report : GSP Evaluation Final Report – Main Report Jan 2024 (5713k)
- Final Report – Annex : GSP Evaluation Final Report – Appendices Jan 2024 (4383k)
- Other : GSP Evaluation Final Report – Policy Briefing Jan 2024 (1087k)
- Summary Report : GSP Evaluation Final Report – Summary Jan 2024 (1149k)
You can also find a pair of infographics and two slide decks summarising the results of the evaluation on this page of the blog Green Social Prescribing Test and Learn Pilots Evaluation Reports, Slide-decks and Infographics | Beyond Greenspace
The main outputs can also be found on Defra’s Evidence portal. In early 2023 the Interim results were published.
What we found
Outcomes for people with mental health needs
Overall, 8,339 people with mental health needs were supported to access nature-based activities through the seven GSP Project Test and Learn pilots. A broader range of people compared to many other social prescribing initiatives, were involved, including children and young people aged under 18, ethnic minority populations (21%), and people from socio-economically deprived areas (57% in IMD deciles 1-3). These participants experienced improved wellbeing when accessing naturebased activities, indicating that GSP can have a positive impact.
“After the group I feel joyful, happy, calm. I have a sense of achievement and I feel my wellbeing increasing. I look forward to attending.”
“It works better than medication for me. It works better than CBT for me. Most of my stuff is related to trauma, so NICE guidelines don’t recommend medication for borderline personality disorder. I have my counselling and that is really valuable, but this is on a par with that.”
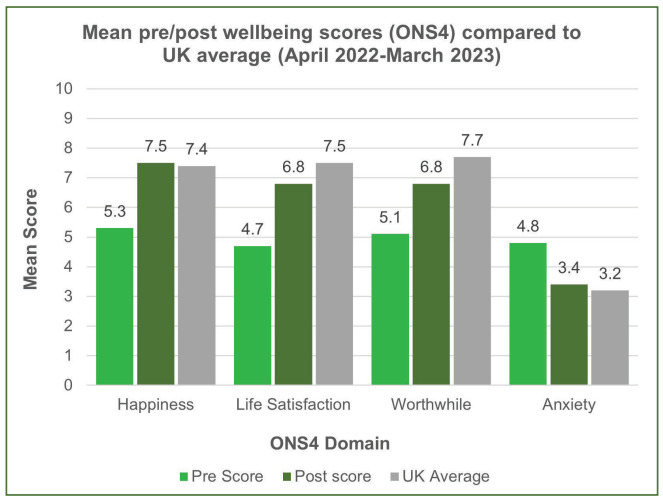
Across the seven pilots there was a statistically significant improvement in wellbeing for each of the ONS4 wellbeing domains after accessing nature-based activities through the GSP Project. Prior to accessing nature-based activities participants’ happiness, anxiety, life satisfaction and feeling that their life was worthwhile was much worse than the national average. After accessing nature-based activities this had improved so that their happiness and anxiety was in line with the national average, and the gap to the national average for levels of life satisfaction and feeling that their life was worthwhile had narrowed
significantly.
Cost effectiveness of GSP
Although a full cost benefit analysis has not been attempted due to the complexity of the GSP projects and the limitations and partiality of the data, the average cost per participant engaged in nature-based activities was £507. This means that compared with other mental health interventions such as behavioural activation, Cognitive Behavioural Therapy (CBT), early intervention for psychosis and collaborative care for depression, nature-based activities are a relatively cost-efficient way to support people across a wide spectrum of mental health needs.
WELLBYs were used to estimate the value of improvements in individual life satisfaction experienced following participation in nature-based activities. The central estimated value of WELLBYs created through the GSP Project was £14.0 million. The estimated (social) return on investment of the GSP project was £1.88 for every £1 invested by the HM Treasury Shared Outcomes Fund, national partners and local test and learn sites.
How to scale and spread Green Social Prescribing
Nature-based activities are complex interventions, operating within the complex social prescribing system. The GSP Project took place against a backdrop of other challenges, such as the COVID-19 pandemic, cost of living crisis, pressures within the NHS and structural shifts to establish ICBs/ICSs. Scaling up and embedding in this context and with multiple partners and operating models is challenging, especially in a short timeline. We used a Realist informed method to explore how GSP can be successfully embedded in localities to tackle and prevent mental ill-health:
- There is a need for new commissioning and procurement arrangements to ensure that nature-based providers can be embedded within health service delivery and the wider social prescribing landscape.
- When political and strategic influence is directed to support GSP it can lead to shifts in policy and budgeting.
- It is necessary to grow and develop naturebased providers to ensure there are a range of appropriate, diverse, geographically spread GSP opportunities.
- There is a need to remove barriers and create aligned structures, to ensure coherence and clarity of roles and responsibilities across the system.
- Improvements to the gathering and sharing of data about GSP outputs and outcomes are necessary to build confidence in the efficacy of GSP.
- There is a need to improve information flow and feedback loops between providers, Link Workers (LWs), referrers and funders to create more efficient and effective pathways.
- Mutual accountability and shared problem-solving is necessary to enhance service users’ experiences, but this requires trust and respect so that people understand and are aware of how different actors in the system may operate.
- Building referrers’ capability, opportunity and motivation to refer to GSP will improve access to appropriate green opportunities.
- Equitable access to appropriate green opportunities requires decision making through an inequalities and instructional lens
- User voice can ensure green social prescribing is person-centred by illuminating the changes needed across the pathway.
- Ensuring service users have a positive experience across the GSP pathway is vital if numbers of referrals are to increase.
In addition to the key fundings above, we also found that:
- The role of the GSP T&L Project Manager was pivotal in providing leadership and influencing local culture and is likely necessary in any system.
- Approaches to link up and build understanding and trust between different parts of the system were key, as well as supporting or establishing networks for nature-based providers.
- Key challenges remain around short term funding cycles for VCSE nature-based delivery, particularly for smaller organisations. Investment and funding, including commissioning and procurement arrangements, remains a critical issue to ensure longevity of progress and appropriate levels of support for VCSE groups.
- Agreeing, establishing, and resourcing data systems that can best capture movement of people through the GSP system, understand drop-out, and provide robust evidence of impact on participants remains a challenge but needs to be tackled.
Background to the evaluation of the Preventing and Tackling Mental Ill Health through Green Social Prescribing Project
| What is Green Social Prescribing? In this project, green social prescribing (GSP) is the practice of supporting people to engage in nature-based interventions and activities to improve their mental health. Social prescribing Link Workers (and other trusted professionals in allied roles) connect people to community groups and agencies for practical and emotional support, based on a ‘what matters to you’ conversation. There are four ‘pillars’ of social prescribing that Link Workers connect to: physical activities, arts/cultural activities, debt and other practical advice, and nature-based activities. There are many different types of nature-based activities and therapies that people may reach through a social prescription and include: conservation and other hands-on practical environmental activities; horticulture and gardening; care farming; walking and other exercise groups in nature; and more formal talking therapies based in the outdoors. |
The government invested over £5.7m to better understand how nature can be used to improve mental health and wellbeing. Seven pilots were selected for Phase 1:
- Humber Coast and Vale Health and Care Partnership
- South Yorkshire and Bassetlaw Integrated Care System
- Nottingham and Nottinghamshire Integrated Care System
- Joined Up Care Derbyshire Sustainability and Transformation Partnership
- Greater Manchester Health & Social Care Partnership
- Surrey Heartlands Health and Care Partnership
- Bristol, North Somerset and South Gloucestershire Sustainability and Transformation Partnership
The initial phase of the Preventing and Tackling Mental Ill Health through Green Social Prescribing Project was completed in Summer 2023, a new round of funding has been awarded to the sites to further develop and embedd progress made in Phase 1. The evaluation team are also working on this second phase with results expected in late 2025.
As an evaluation team, we have taken a whole systems, realist informed approach and worked towards an understanding of how green social prescribing could be scaled up and embedded into practice effectively. The evaluation of the test and learn pilots was funded for a total of £887,413 from HMT’s Shared Outcomes Fund, a fund announced by HM Treasury to pilot innovative ways of working that will improve collaboration on priority policy areas that sit across, and are delivered by, multiple public sector organisations to improve outcomes and deliver better value for citizens. The evaluation contract was awarded by the Department for Environment Food and Rural Affairs (Defra), and will be supported by Department of Health and Social Care (DHSC), Natural England, NHS England, Public Health England (now OHID), Sport England, the National Academy of Social Prescribing (NASP), and the Ministry of Housing, Communities and Local Government (MHCLG).
Haywood, A., Dayson, C., Garside, R., Foster, A., Lovell, R., Husk, K., Holding, E., Thompson, J., Shearn, K., Hunt, H.A., Dobson, J., Harris, C., Jacques, R., Witherley, D., Northall, P., Baumann, M., Wilson, I,. National Evaluation of the Preventing and Tackling Mental Ill Health through Green Social Prescribing Project: Final Report. January 2024. Department for Environment, Food and Rural Affairs (London).
This report, and the accompanying briefing, summary and appendices documents, are published by Defra (Defra Project Code BE0191) and are available from the Department’s Science and Research Projects Database at https://randd.defra.gov.uk. Whilst the research was commissioned by Defra, the views expressed reflect the evaluation findings and the authors’ interpretation; they do not necessarily reflect
Defra policy.